Non Surgical Treatment For Hammer Toes
 Overview
Overview
Hammer toes a bending and hardening of the joints of the second, third, fourth, or fifth toes. If you look down at your feet and you can?t see the tips of the toenails, you might suffer from hammertoe. Early signs of hammertoe are a bend in the joint of any toe except the big toe. The bend in the joint causes the top of the toe to appear to curl under as if it?s ?hammering? into the floor.
Causes
Many people develop hammertoe because they wear shoes that are too tight. Shoes with narrow toe boxes squeeze the toes together, forcing some to bend. This causes the toe muscles to contract. If the toes are forced into this cramped position too often, the muscles may permanently tighten, preventing the toes from extending. Chronic hammertoe can also hammertoe cause the long bones that connect the toes to the foot, called metatarsals, to move out of position. The misaligned metatarsal bones may pinch a nerve running between them, which can cause a type of nerve irritation called a neuroma.
 Symptoms
Symptoms
The most obvious symptom of hammertoe is the bent, hammer-like or claw-like appearance of one or more of your toes. Typically, the proximal joint of a toe will be bending upward and the distal joint will be bending downward. In some cases, both joints may bend downward, causing the toes to curl under the foot. In the variation of mallet toe, only the distal joint bends downward. Other symptoms may include Pain and stiffness during movement of the toe, Painful corns on the tops of the toe or toes from rubbing against the top of the shoe's toe box, Painful calluses on the bottoms of the toe or toes, Pain on the bottom of the ball of the foot, Redness and swelling at the joints. If you have any of these symptoms, especially the hammer shape, pain or stiffness in a toe or toes, you should consider consulting your physician. Even if you're not significantly bothered by some of these symptoms, the severity of a hammertoe can become worse over time and should be treated as soon as possible. Up to a point hammertoes can be treated without surgery and should be taken care of before they pass that point. After that, surgery may be the only solution.
Diagnosis
Your healthcare provider will examine your foot, checking for redness, swelling, corns, and calluses. Your provider will also measure the flexibility of your toes and test how much feeling you have in your toes. You may have blood tests to check for arthritis, diabetes, and infection.
Non Surgical Treatment
Inserts in your shoes can be used to help relieve pressure on the toes from the deformity. Splints/Straps. These can be used to help re-align and stretch your toes and correct the muscle imbalance and tendon shortening. One of the most common types are toe stretchers like the yogatoe. Chiropody. A chiropodist can remove calluses or corns, areas of hard skin that have formed to make the foot more comfortable.Steroid injections can help to reduce pain and inflammation.
Surgical Treatment
Surgery is used when other types of treatment fail to relieve symptoms or for advanced cases of hammertoe. There are several types of surgeries to treat hammertoe. A small piece of bone may be removed from the joint (arthroplasty). The toe joint may be fused to straighten it (arthrodesis). Surgical hardware, such as a pin, may be used to hold the bones in place while they heal. Other types of surgery involve removing skin (wedging) or correcting muscles and tendons to balance the joint.
 Prevention
Prevention
Prevention of a hammer toe can be difficult as symptoms do not usually start until the problem is well established. Wearing shoes that have extra room in the toes may help the problem or slow down its development.
Will Over-Pronation Need An Operation
Over-pronation is very common and affects millions of people. To better understand this condition, we'll take a closer look at the 3 most common foot types. An estimated 70% of the population has fallen arches (or a low arch). Only 20% has a normal arch. And 10% have abnormal feet, in other words they either have flat feet or the opposite a high arched foot.

Causes
Over-pronation may happen because the tissue that attaches to your foot bones is loose. You may be born with this problem or it may result from injuries or overuse, like from too much running.
Symptoms
Over-pronation is a condition where the arch flattens out which makes the feet roll inward while walking. This condition is also known as flat feet. It imposes extreme additional stresses on the plantar fascia, a fibrous band of tissue which connects the heel to the forefoot. Over-pronation makes walking a painful experience because of the additional strain on the calves, heel and/or back. Treatment for over-pronation involves the use of specially-made orthotics which offers arch support and medial rear foot posting as corrective measures.
Diagnosis
The best way to discover whether you have a normal gait, or if you overpronate, is to visit a specialty run shop, an exercise physiologist, a podiatrist or a physical therapist who specializes in working with athletes. A professional can analyze your gait, by watching you either walk or run, preferably on a treadmill. Some facilities can videotape your gait, then analyze the movement of your feet in slow-motion. Another (and less costly) way is to look at the bottom of an older pair of run shoes. Check the wear pattern. A person with a normal gait will generally see wear evenly across the heel and front of the shoe. A person who overpronates will likely see more wear on the OUTside of the heel and more wear on the INside of the forefoot (at the ball). A person who supinates will see wear all along the outer edges of the shoe. You can also learn about your gait by looking at your arches. Look at the shape your wet feet leave on a piece of paper or a flat walking surface.
Non Surgical Treatment
Over-Pronation can be treated conservatively (non-surgical treatments) with over-the-counter orthotics. These orthotics should be designed with appropriate arch support and medial rearfoot posting to prevent the over-pronation. Footwear should also be examined to ensure there is a proper fit. Footwear with a firm heel counter is often recommended for extra support and stability. Improperly fitting footwear can lead to additional foot problems.
Surgical Treatment
Depending on the severity of your condition, your surgeon may recommend one or more treatment options. Ultimately, however, it's YOUR decision as to which makes the most sense to you. There are many resources available online and elsewhere for you to research the various options and make an informed decision.
Severs Disease Physical Therapy
If your child is experiencing activity related pain just below the kneecap, at the top of the shinbone, or in their heel or hip then the chances are they are suffering from Osgood Schlatter, Severs disease or Ischial Apophysitis respectively. Today, thousands of children are diagnosed with one of these conditions every year. Many others are never diagnosed and the discomfort is often dismissed as 'growing pains'
Causes
Your child is most at risk for this condition when he or she is in the early part of the growth spurt in early puberty. Sever's disease is most common in physically active girls 8 years to 10 years of age and in physically active boys 10 years to 12 years of age. Soccer players and gymnasts often get Sever's disease, but children who do any running or jumping activity may also be at an increased risk. Sever's disease rarely occurs in older teenagers because the back of the heel has typically finished growing by 15 years of age.
Symptoms
The most obvious sign of Sever's disease is pain or tenderness in one or both heels, usually at the back. The pain also might extend to the sides and bottom of the heel, ending near the arch of the foot. A child also may have these related problems, swelling and redness in the heel, difficulty walking, discomfort or stiffness in the feet upon awaking, discomfort when the heel is squeezed on both sides, an unusual walk, such as walking with a limp or on tiptoes to avoid putting pressure on the heel. Symptoms are usually worse during or after activity and get better with rest.
Diagnosis
A physical exam of the heel will show tenderness over the back of the heel but not in the Achilles tendon or plantar fascia. There may be tightness in the calf muscle, which contributes to tension on the heel. The tendons in the heel get stretched more in patients with flat feet. There is greater impact force on the heels of athletes with a high-arched, rigid foot. The doctor may order an x-ray because x-rays can confirm how mature the growth center is and if there are other sources of heel pain, such as a stress fracture or bone cyst. However, x-rays are not necessary to diagnose Sever?s disease, and it is not possible to make the diagnosis based on the x-ray alone.
Non Surgical Treatment
First, your child should cut down or stop any activity that causes heel pain. Apply ice to the injured heel for 20 minutes 3 times a day. If your child has a high arch, flat feet or bowed legs, your doctor may recommend orthotics, arch supports or heel cups. Your child should never go barefoot. If your child has severe heel pain, medicines such as acetaminophen (one brand name: Tylenol) or ibuprofen (some brand names. Advil, Motrin, Nuprin) may help.
Prevention
The best way to prevent Sever's disease is to make sure that your child wears shoes that fit properly. The heel portion of the shoe should not be too tight, and there should be good padding in the heel. It may help to put extra heel pads in your child's shoes. Some children simply get too much physical activity. For example, they may play on too many teams or practice for too long. Their heel pain is a message to slow down.
The Cause And Treatment Of Posterior Tibial Tendon Dysfunction (PTTD)
Overview
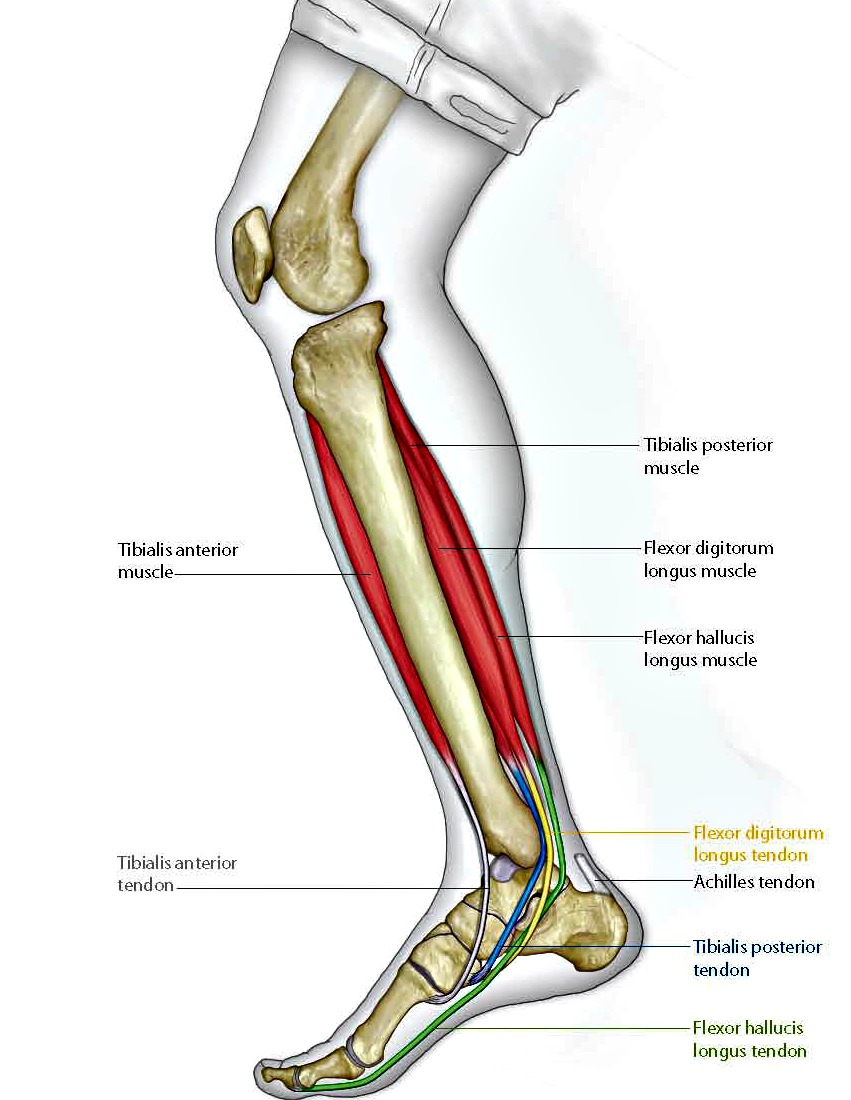
Over 60 Million Americans suffer from Adult Acquired Flatfoot (AAF), otherwise known as Posterior Tibial Tendon Dysfunction or PTTD. This condition generally occurs in adults from 40-65 years of age, and it usually only occurs in one foot, not both. The Posterior Tibial (PT) Tendon courses along the inside part of the ankle and underneath the arch of the foot. It is the major supporting structure for the arch. Over time, the tendon becomes diseased, from overuse, and starts to lose it's strength. As a result, the arch begins to collapse, placing further strain on the PT Tendon, leading to further decrease in tendon strength, which causes further collapse of the arch. This is described as a progressive deformity because it will generally get worse over time. 
Causes
Posterior tibial tendon dysfunction is the most common cause of acquired adult flatfoot. Sometimes this can be a result of specific trauma, but usually the tendon becomes injured from wear and tear over time. This is more prevalent in individuals with an inherited flat foot but excessive weight, age, and level of activity are also contributing factors.
Symptoms
Symptoms of pain may have developed gradually as result of overuse or they may be traced to one minor injury. Typically, the pain localizes to the inside (medial) aspect of the ankle, under the medial malleolus. However, some patients will also experience pain over the outside (lateral) aspect of the hindfoot because of the displacement of the calcaneus impinging with the lateral malleolus. This usually occurs later in the course of the condition. Patients may walk with a limp or in advanced cases be disabled due to pain. They may also have noticed worsening of their flatfoot deformity.
Diagnosis
First, both feet should be examined with the patient standing and the entire lower extremity visible. The foot should be inspected from above as well as from behind the patient, as valgus angulation of the hindfoot is best appreciated when the foot is viewed from behind. Johnson described the so-called more-toes sign: with more advanced deformity and abduction of the forefoot, more of the lateral toes become visible when the foot is viewed from behind. The single-limb heel-rise test is an excellent determinant of the function of the posterior tibial tendon. The patient is asked to attempt to rise onto the ball of one foot while the other foot is suspended off the floor. Under normal circumstances, the posterior tibial muscle, which inverts and stabilizes the hindfoot, is activated as the patient begins to rise onto the forefoot. The gastrocnemius-soleus muscle group then elevates the calcaneus, and the heel-rise is accomplished. With dysfunction of the posterior tibial tendon, however, inversion of the heel is weak, and either the heel remains in valgus or the patient is unable to rise onto the forefoot. If the patient can do a single-limb heel-rise, the limb may be stressed further by asking the patient to perform this maneuver repetitively.
Non surgical Treatment
Get treated early. There is no recommended home treatment. While in stage one of the deformity, rest, a cast, and anti-inflammatory therapy can help you find relief. This treatment is followed by creating custom-molded foot orthoses and orthopedic footwear. These customized items are critical in maintaining the stability of the foot and ankle. Once the tendon has stretched and deformity is visible, the chances of success for non-surgical treatment are significantly lower. In a small percentage of patients, total immobilization may arrest the progression of the deformity. A long-term brace known as an ankle foot orthosis is required to keep the deformity from progressing. The Richie Brace, a type of ankle foot orthosis, shows significant success as a treatment for stage two posterior tibial dysfunction. It is a sport-style brace connected to a custom corrected foot orthodic that fits into most lace-up footwear (including athletic shoes). It is also light weight and more cosmetically appealing than traditionally prescribed ankle foot orthosis. The Arizona Brace, California Brace or Gauntlet Brace may also be recommended depending on your needs. 
Surgical Treatment
Stage two deformities are less responsive to conservative therapies that can be effective in mild deformities. Bone procedures are necessary at this stage in order to recreate the arch and stabilize the foot. These procedures include isolated fusion procedures, bone grafts, and/or the repositioning of bones through cuts called osteotomies. The realigned bones are generally held in place with screws, pins, plates, or staples while the bone heals. A tendon transfer may or may not be utilized depending on the condition of the posterior tibial tendon. Stage three deformities are better treated with surgical correction, in healthy patients. Patients that are unable to tolerate surgery or the prolonged healing period are better served with either arch supports known as orthotics or bracing such as the Richie Brace. Surgical correction at this stage usually requires fusion procedures such as a triple or double arthrodesis. This involves fusing the two or three major bones in the back of the foot together with screws or pins. The most common joints fused together are the subtalar joint, talonavicular joint, and the calcaneocuboid joint. By fusing the bones together the surgeon is able to correct structural deformity and alleviate arthritic pain. Tendon transfer procedures are usually not beneficial at this stage. Stage four deformities are treated similarly but with the addition of fusing the ankle joint.
Arch Pain Triggers Signs Or Symptoms And Treatment Procedures
Arch pain is common in people with a typical structural problem known as flat feet. Arch pain may also occur in people with fallen arches (a fallen arch is one that has collapsed due to bearing weight). Flat feet can lead to extreme stress or inflammation of the plantar fascia, possibly causing severe discomfort and leading to other foot problems. Without properly supported arches, simple movement can pull your body out of alignment and cause stress, strain and fatigue to your lower body.

Causes
A common cause of foot arch pain is a stress fracture. They tend to occur from repeated overloading of one of the foot bones from activities such as jumping and running especially if you have suddenly increased your activity level. The breaks in the bone may be small but they can be extremely painful. Stress fractures of the metatarsal bones or the navicular can cause anything from mild to severe foot arch pain. The Tibialis Posterior muscle plays a very important role in supporting the medial arch of the foot. Posterior Tibial Tendonitis can occur either through repetitive use e.g. high impact sports such as soccer or tennis, or from an injury e.g. a fall. This causes the tendon to become inflamed or even torn, resulting in pain on bottom of foot. This pain usually gets worse with activity or when standing for long periods. If the problem persists, the inner side of the foot (known as the medial longitudinal arch of the foot) gradually collapses down, causing flat feet. A simple test for this condition is to stand on one leg and rise up onto your tiptoes. If you cannot, it indicates a problem with the Posterior Tibial tendon. Treatment usually consists of rest, ice, exercises, orthotics and physical therapy.
Symptoms
Pain in arch of foot is really the only symptom of this condition. It is unlikely to see any swelling or bruising and instead there will be a deep tender spot near the heel. Occasionally the pain may radiate further down the foot. With this condition, pain will usually be felt first thing in the morning or after periods of sitting. This is because the plantar fascia tightens and shortens slightly when there is no weight on it and by standing on it it suddenly stretches and becomes painful. After a few steps it starts to loosen off and the pain may subside. If this is the same pattern of pain you experience it is quite likely you have plantar fasciits. Pain may also be felt when walking up stairs or standing on tip-toes (anything that stretches the fascia).
Diagnosis
The doctor will take a brief history to determine how the injury occurred. If necessary, a thorough physical exam may be conducted to evaluate for any other injuries. Taking your workout shoes to the exam may also provide valuable information to the medical practitioner. Both feet will be physically and visually examined by the medical practitioner. The foot and arch will be touched and manipulated possibly with a lot of pressure and inspected to identify obvious deformities, tender spots, or any differences in the bones of the foot and arch.
Non Surgical Treatment
If it is flat feet, then you'd seek professional advice and maybe need orthotics, or arch supports to prevent the pressures and to stop the pain. One of the other reasons you can get pain in this area of the foot is plantar fasciitis. The plantar fascia is a membrane that is inside of the skin and attaches to the heel bone here. It divides into three bands that go out of the foot here: the outer band, the central band, and the medial band here. Often, from impact, you get an inflammation of that attachment to the heel bone and this can often spread up the medial band and this is another way of getting pain in that arch. Now, the way to treat that is also using arch supports but also heel cushions, better soled shoes to prevent the pressure. These things normally disappear after a year, 18 months. Plantar fasciitis is easier to treat because it's not a long term problem. If you do need arch support, something like this would be very good for both problems.

Surgical Treatment
There are two types of bone procedure for flat feet, those where bone cuts and bone grafts are used to alter the alignment by avoiding any joint structures, or joint invasive procedures (called fusions or arthrodeses) that remove a joint to reshape the foot. With joint fusion procedures, there are those procedures that involve non-essential joints of the foot versus those that involve essential joints. All bone procedures have their place in flat foot surgery, and Dr. Blitz carefully evaluates each foot to preserve as much motion and function while obtaining proper and adequate alignment. In many cases a flat foot reconstruction involves both soft tissue procedures and bone procedures to rebuild and restore the arch. There are several joints in the arch of the foot that can collapse - and these joints are non-essential joints of the foot. This does not mean that they do not have a purpose, but rather become inefficient is providing a stable platform for function. As such, locking these non-essential non-functioning joints into place is commonly recommended. These joints are fused together with screws and/or plates. A heel bone that is no longer in proper position and pushed outwards away from the foot can be corrected with a bone cut and realignment procedure, so long as the displacement is not too significant. A benefit of this surgery is that it keeps the back portion of the foot mobile, and helps the surrounding tendons work for efficiently in maintaining the arch. In certain flat feet, the foot is deviated outwards and away from the midline of the body. Sometimes, this is due to the outer portion of the foot being shorter than the inner portion. Here bone graft can be added to the outer edge of the foot to lengthen the foot to swing the foot over into a corrected position. This procedure is most commonly performed in children and young adults. A bone graft is inserted into the top part of the arch to realign a component of the flat foot, medically known as forefoot varus or medial column elevatus. The back part of the foot (called the rearfoot complex) can be the cause (or source) of the flat foot or the simply affected by the flat foot foot. In simple terms, the back part of the foot can be made to flatten out due to arch problems - and vica versa for that matter. Dr. Blitz specifically identifies the cause of the flat foot as this will determine the best treatment plan, as each flat foot needs to be evaluated individually. The rearfoot is made up of three joints, and depending on the extent and most importantly the rigidity of these joints, they may require fusion to restore alignment. When all three joints require fusion - this call is a triple arthrodesis. For completeness, isolated fusion of any of the three joints can be performed (such as subtalar joint arthrodesis, talonavicular arthrodesis, and calcaneaocuboid joint arthrodesis). The medical decision making for isolated fusions is beyond the scope this article, but Dr. Blitz tries to avoid any rearfoot fusion for flexible feet because these are joints are essential joints of the foot, especially in younger people. Those in severe cases, it may be advantageous to provide re-alignment.
Prevention
To prevent arch pain, it is important to build up slowly to your exercise routine while wearing arch supports inside training shoes. By undertaking these simple measures you can prevent the discomfort of arch pain which can otherwise linger for many months. While you allow the foot to recover, it will help to undertake low impact exercises (such as swimming or water aerobics).
Stretching Exercises
Below are two simple plantar fasciitis stretching exercises to help improve the flexibility of the muscles and tendons around the foot and ankle. Plantar fasciitis stretch taken from The Stretching Handbook. Kneel on one foot and place your body weight over your knee. Keep your heel on the ground and lean forward. In the photo to the left, the athlete is stretching the arch of her left foot. Kneel on one foot with your hands on the ground. Place your body weight over your knee and slowly move your knee forward. Keep your toes on the ground and arch your foot. In the photo to the right, the athlete is stretching the arch of his right foot.
Causes Signs Or Symptoms And Therapy For An Achilles Tendon Rupture
Overview  An Achilles tendon rupture is also known as a rupture of the gastrocnemius tendon, or the common calcanean tendon. The tendon is actually composed of 5 different tendons, the two most important being the superficial digital flexor and gastrocnemius tendons. The gastrocnemius tendon is the largest of these, and is the most powerful extensor of the hock (ankle) joint. Both the superficial digital flexor and gastrocnemius tendons attach to the heel bone, called the calcaneus bone. A rupture of the Achilles tendon may be a partial tear, which means just the gastrocnemius is torn, or a complete tear, in which all five tendons have been torn. (show diagrams, normal anatomy vs partial vs complete tears). Causes Your Achilles tendon helps you point your foot downward, rise on your toes and push off your foot as you walk. You rely on it virtually every time you move your foot. Rupture usually occurs in the section of the tendon located within 2 1/2 inches (about 6 centimeters) of the point where it attaches to the heel bone. This section may be predisposed to rupture because it gets less blood flow, which also may impair its ability to heal. Ruptures often are caused by a sudden increase in the amount of stress on your Achilles tendon. Common examples include increasing the intensity of sports participation, especially in sports that involve jumping, falling from a height, stepping into a hole. Symptoms The most common symptom of Achilles tendonitis is a sudden surge of pain in the heel and back of the ankle at the point of injury which is often described as a snapping sensation in the heel. After the injury has occurred, patients then struggle or find it near impossible to bear any weight on the affected leg. Pain can often be most prominent first thing in the morning after the injury has been rested. Swelling and tenderness is also likely to appear in the area. Diagnosis In diagnosing an Achilles tendon rupture, the foot and ankle surgeon will ask questions about how and when the injury occurred and whether the patient has previously injured the tendon or experienced similar symptoms. The surgeon will examine the foot and ankle, feeling for a defect in the tendon that suggests a tear. Range of motion and muscle strength will be evaluated and compared to the uninjured foot and ankle. If the Achilles tendon is ruptured, the patient will have less strength in pushing down (as on a gas pedal) and will have difficulty rising on the toes. The diagnosis of an Achilles tendon rupture is typically straightforward and can be made through this type of examination. In some cases, however, the surgeon may order an MRI or other advanced imaging tests. Non Surgical Treatment Achilles tendon ruptures can be treated non-operatively or operatively. Both of these treatment approaches have advantages and disadvantages. In general, younger patients with no medical problems may tend to do better with operative treatment, whereas patients with significant medical problems or older age may be best served with non-operative treatment. However, the decision of how the Achilles tendon rupture is treated should be based on each individual patient after the advantages and disadvantages of both treatment options are reviewed. It is important to realize that while Achilles tendon ruptures can be treated either non-operatively or operatively, they must be treated. A neglected Achilles tendon rupture (i.e. one where the tendon ends are not kept opposed) will lead to marked problems of the leg in walking, which may eventually lead to other limb and joint problems. Furthermore, late reconstruction of non-treated Achilles tendon rupture is significantly more complex than timely treatment.
An Achilles tendon rupture is also known as a rupture of the gastrocnemius tendon, or the common calcanean tendon. The tendon is actually composed of 5 different tendons, the two most important being the superficial digital flexor and gastrocnemius tendons. The gastrocnemius tendon is the largest of these, and is the most powerful extensor of the hock (ankle) joint. Both the superficial digital flexor and gastrocnemius tendons attach to the heel bone, called the calcaneus bone. A rupture of the Achilles tendon may be a partial tear, which means just the gastrocnemius is torn, or a complete tear, in which all five tendons have been torn. (show diagrams, normal anatomy vs partial vs complete tears). Causes Your Achilles tendon helps you point your foot downward, rise on your toes and push off your foot as you walk. You rely on it virtually every time you move your foot. Rupture usually occurs in the section of the tendon located within 2 1/2 inches (about 6 centimeters) of the point where it attaches to the heel bone. This section may be predisposed to rupture because it gets less blood flow, which also may impair its ability to heal. Ruptures often are caused by a sudden increase in the amount of stress on your Achilles tendon. Common examples include increasing the intensity of sports participation, especially in sports that involve jumping, falling from a height, stepping into a hole. Symptoms The most common symptom of Achilles tendonitis is a sudden surge of pain in the heel and back of the ankle at the point of injury which is often described as a snapping sensation in the heel. After the injury has occurred, patients then struggle or find it near impossible to bear any weight on the affected leg. Pain can often be most prominent first thing in the morning after the injury has been rested. Swelling and tenderness is also likely to appear in the area. Diagnosis In diagnosing an Achilles tendon rupture, the foot and ankle surgeon will ask questions about how and when the injury occurred and whether the patient has previously injured the tendon or experienced similar symptoms. The surgeon will examine the foot and ankle, feeling for a defect in the tendon that suggests a tear. Range of motion and muscle strength will be evaluated and compared to the uninjured foot and ankle. If the Achilles tendon is ruptured, the patient will have less strength in pushing down (as on a gas pedal) and will have difficulty rising on the toes. The diagnosis of an Achilles tendon rupture is typically straightforward and can be made through this type of examination. In some cases, however, the surgeon may order an MRI or other advanced imaging tests. Non Surgical Treatment Achilles tendon ruptures can be treated non-operatively or operatively. Both of these treatment approaches have advantages and disadvantages. In general, younger patients with no medical problems may tend to do better with operative treatment, whereas patients with significant medical problems or older age may be best served with non-operative treatment. However, the decision of how the Achilles tendon rupture is treated should be based on each individual patient after the advantages and disadvantages of both treatment options are reviewed. It is important to realize that while Achilles tendon ruptures can be treated either non-operatively or operatively, they must be treated. A neglected Achilles tendon rupture (i.e. one where the tendon ends are not kept opposed) will lead to marked problems of the leg in walking, which may eventually lead to other limb and joint problems. Furthermore, late reconstruction of non-treated Achilles tendon rupture is significantly more complex than timely treatment.  Surgical Treatment Surgery will involve stitching the two ends of the tendon together, before placing the leg in a cast or brace. The advantage of having an operation is the reduced chance of the rupture reoccurring, however it will involve the risks associated with any surgical procedure, such as infection. Prevention To help reduce your chance of getting Achilles tendon rupture, take the following steps. Do warm-up exercises before an activity and cool down exercises after an activity. Wear proper footwear. Maintain a healthy weight. Rest if you feel pain during an activity. Change your routine. Switch between high-impact activities and low-impact activities. Strengthen your calf muscle with exercises.
Surgical Treatment Surgery will involve stitching the two ends of the tendon together, before placing the leg in a cast or brace. The advantage of having an operation is the reduced chance of the rupture reoccurring, however it will involve the risks associated with any surgical procedure, such as infection. Prevention To help reduce your chance of getting Achilles tendon rupture, take the following steps. Do warm-up exercises before an activity and cool down exercises after an activity. Wear proper footwear. Maintain a healthy weight. Rest if you feel pain during an activity. Change your routine. Switch between high-impact activities and low-impact activities. Strengthen your calf muscle with exercises.
The Treatment And Cause Of Achilles Tendon Pain
 Achilles tendinitis is an overuse injury common in many sports that require lots of running and jumping. Once this condition becomes more chronic adhesions that form along the tissues and the injury becomes more of a tendinosis. Treatment for a tendinosis is much different that for a tendinitis, so it is important to recognize what stage the injury is at in order to treat it appropriately. An acute achilles tendinitis involves inflammation and would be treated with rest, ice, etc. Once the inflammation has decreased, research shows that eccentric exercises are beneficial. Once there is tendinosis, it becomes imperative to break up those adhesions with ART and prescribe appropriate stretches and exercises.
Achilles tendinitis is an overuse injury common in many sports that require lots of running and jumping. Once this condition becomes more chronic adhesions that form along the tissues and the injury becomes more of a tendinosis. Treatment for a tendinosis is much different that for a tendinitis, so it is important to recognize what stage the injury is at in order to treat it appropriately. An acute achilles tendinitis involves inflammation and would be treated with rest, ice, etc. Once the inflammation has decreased, research shows that eccentric exercises are beneficial. Once there is tendinosis, it becomes imperative to break up those adhesions with ART and prescribe appropriate stretches and exercises.
Causes
As ?overuse? disorders, Achilles tendonitis and tendonosis are usually caused by a sudden increase of a repetitive activity involving the Achilles tendon. Such activity puts too much stress on the tendon too quickly, leading to micro-injury of the tendon fibers. Due to this ongoing stress on the tendon, the body is unable to repair the injured tissue. The structure of the tendon is then altered, resulting in continued pain. Achilles4Athletes are at high risk for developing disorders of the Achilles tendon. Achilles tendonitis and tendonosis are also common in individuals whose work puts stress on their ankles and feet, such as laborers, as well as in ?weekend warriors?-those who are less conditioned and participate in athletics only on weekends or infrequently. In addition, people with excessive pronation (flattening of the arch) have a tendency to develop Achilles tendonitis and tendonosis due to the greater demands placed on the tendon when walking. If these individuals wear shoes without adequate stability, their over-pronation could further aggravate the Achilles tendon.
Symptoms
Achilles tendinitis symptoms present as mild to severe pain or swelling near the ankle. The pain may lead to weakness and decreased mobility, symptoms that increase gradually while walking or running. Over time, the pain worsens, and stiffness in the tendon may be noted in the morning. Mild activity may provide relief. Physical exam may reveal an audible cracking sound when the Achilles tendon is palpated. The lower leg may exhibit weakness. A ruptured or torn Achilles tendon is severely painful and warrants immediate medical attention. The signs of a ruptured or torn Achilles tendon include. Acute, excruciating pain. Impaired mobility, unable to point the foot downward or walk on the toes. Weight bearing or walking on the affected side is not possible.
Diagnosis
If Achilles tendonitis is suspected, avoid any exercise or activity that causes the pain. It is advisable to see a doctor promptly so that an accurate diagnosis can be made and appropriate treatment recommended. The doctor will take a full medical history and will ask about the nature and duration of the symptoms. They will perform a physical examination of the affected area. Ultrasound scanning may be used to assess damage to the tendon or surrounding structures. Occasionally MRI (magnetic resonance imaging) may be recommended. The symptoms of Achilles tendonitis are often similar to symptoms of other conditions such as partial Achilles tendon rupture and heel bursitis. This can make diagnosis difficult and a referral to an orthopaedic specialist may be required in order for an accurate diagnosis to be made.
Nonsurgical Treatment
Supportive shoes and orthotics. Pain from insertional Achilles tendinitis is often helped by certain shoes, as well as orthotic devices. For example, shoes that are softer at the back of the heel can reduce irritation of the tendon. In addition, heel lifts can take some strain off the tendon. Heel lifts are also very helpful for patients with insertional tendinitis because they can move the heel away from the back of the shoe, where rubbing can occur. They also take some strain off the tendon. Like a heel lift, a silicone Achilles sleeve can reduce irritation from the back of a shoe. If your pain is severe, your doctor may recommend a walking boot for a short time. This gives the tendon a chance to rest before any therapy is begun. Extended use of a boot is discouraged, though, because it can weaken your calf muscle. Extracorporeal shockwave therapy (ESWT). During this procedure, high-energy shockwave impulses stimulate the healing process in damaged tendon tissue. ESWT has not shown consistent results and, therefore, is not commonly performed. ESWT is noninvasive-it does not require a surgical incision. Because of the minimal risk involved, ESWT is sometimes tried before surgery is considered.

Surgical Treatment
Following the MRI or ultrasound scan of the Achilles tendon the extent of the degenerative change would have been defined. The two main types of operation for Achilles tendinosis are either a stripping of the outer sheath (paratenon) and longitudinal incisions into the tendon (known as a debridement) or a major excision of large portions of the tendon, the defects thus created then being reconstructed using either allograft (donor tendon, such as Wright medical graft jacket) or more commonly using a flexor hallucis longus tendon transfer. In cases of Achilles tendonosis with more minor degrees of degenerative change the areas can be stimulated to repair itself by incising the tendon, in the line of the fibres, which stimulates an ingrowth of blood vessels and results in the healing response. With severe Achilles tendonosis, occasionally a large area of painful tendon needs to be excised which then produces a defect which requires filling. This is best done by transferring the flexor hallucis longus muscle belly and tendon, which lies adjacent to the Achilles tendon. This results in a composite/double tendon after the operation, with little deficit from the transferred tendon.
Prevention
A 2014 study looked at the effect of using foot orthotics on the Achilles tendon. The researchers found that running with foot orthotics resulted in a significant decrease in Achilles tendon load compared to running without orthotics. This study indicates that foot orthoses may act to reduce the incidence of chronic Achilles tendon pathologies in runners by reducing stress on the Achilles tendon1. Orthotics seem to reduce load on the Achilles tendon by reducing excessive pronation,